One day, your periods become irregular. The next month, you wake up drenched in sweat. Then comes insomnia, forgetfulness, and the feeling of losing your footing. What if it wasn't "stress," but the beginning of a new hormonal phase? Perimenopause affects all women, but few know what's going on in their bodies. It's not a breakdown, nor is it inevitable. It's a transition—powerful, complex, and hormonal. So, what's the connection between perimenopause and hormones? In this article, we explain what's really changing and how to navigate this stage mindfully.
Before we talk hormones, what is perimenopause?
Perimenopause is a natural hormonal transition in a woman's life that precedes the infamous menopause. It can begin as early as the late thirties or early forties, although most of us begin to feel its effects around the age of 45. Contrary to popular belief, it's not a sudden event! But a gradual process, often lasting several years.
During this menopausal transition, hormonal fluctuations can be quite dramatic. Yes, the ovaries begin to slow down their hormone production—particularly estrogen and progesterone. But beware: this decline is neither linear nor constant! It occurs in waves, with sometimes confusing phases of variation. This explains why symptoms can appear irregularly and vary from one woman to another.
Perimenopause is the moment when the menstrual cycle begins to go haywire. Menopause (which is the definitive cessation of periods for 12 consecutive months) has not yet set in. Flow becomes more irregular, sometimes heavier. Cycles become more and more spaced out. Some women don't even pay attention to it right away! They attribute the first signs of perimenopause to stress, fatigue, or mental overload.
However, what we feel is not "in the head," but is linked to a hormonal reality. Accepting this phase therefore allows us to better experience it. And it is an essential first step in this transition in women's lives.
What hormones change during perimenopause and how?
Perimenopause is, above all, a hormonal transition. Contrary to the idea of a "dry run" of hormones, it's more of a gradual imbalance—with ups, downs, and roller coasters. We explain which hormones are primarily affected.
Progesterone: the first to decline
The first hormone to kick off hormonal fluctuations? Progesterone. Its decline results in menstrual cycles without ovulation, which become more frequent from the age of forty. However, even though this hormone plays an essential role in regulating the menstrual cycle, it also affects:
- sleep;
- mood
- emotional stability.
So, inevitably, when it is missing... We observe:
- heavier periods;
- anxiety;
- strong irritability;
- lighter sleep.
Often, this drop can go unnoticed in conventional hormonal assessments, because progesterone always fluctuates greatly throughout the cycle.
Estrogens: A roller coaster
Estrogen levels don't drop suddenly: they fluctuate. Some months, their levels are abnormally high, which causes:
- breast pain;
- water retention;
- migraines.
Other times, the rate decrease is drastic, resulting in:
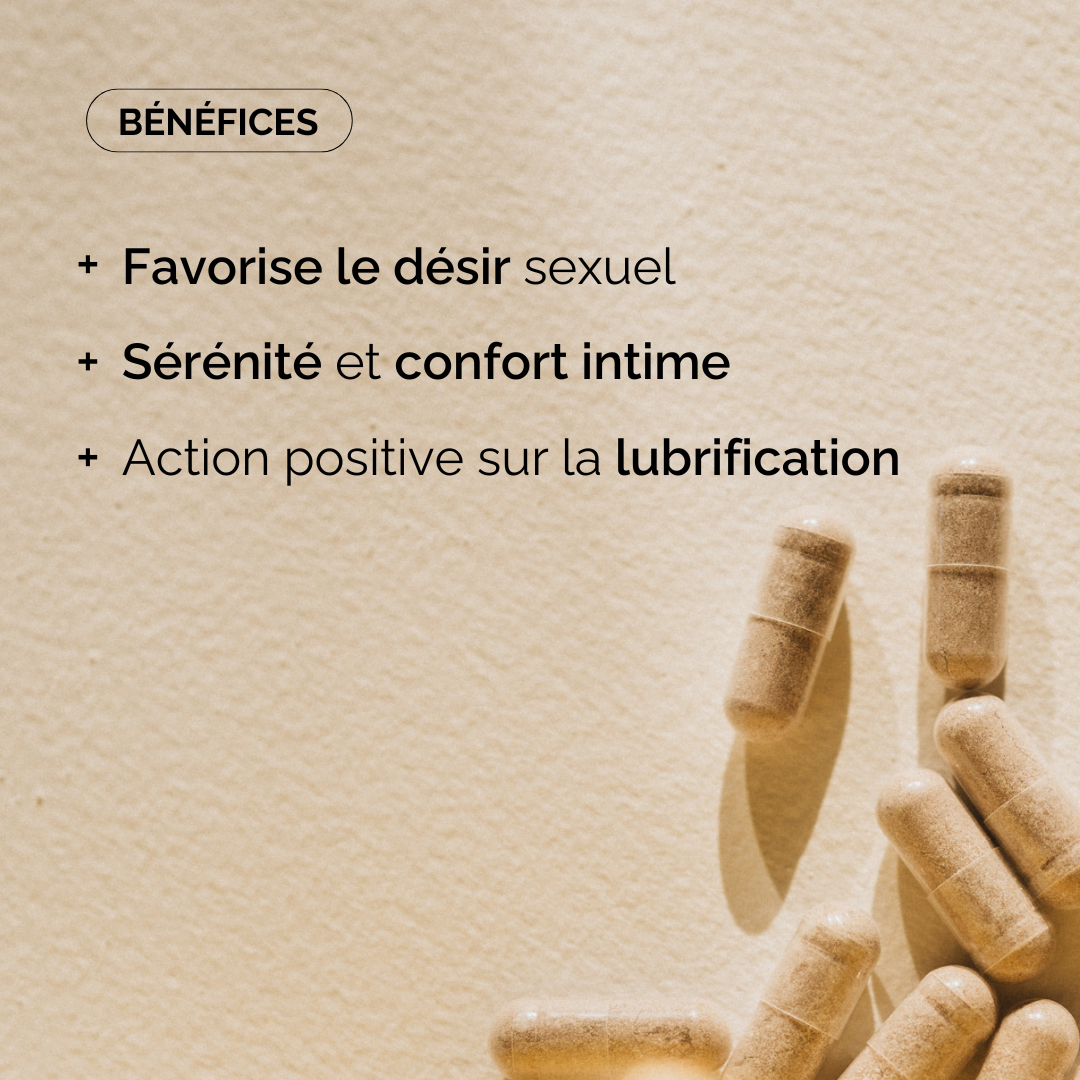
- vaginal dryness;
- night sweats/hot flashes;
- a decrease in libido.
In any case, this hormonal transition makes perimenopause confusing: you feel great one month, then overwhelmed the next. In short, the body tries to compensate, but... it doesn't always find the right balance!
FSH and LH: Hormones That Go Wild
FSH (follicle-stimulating hormone) and LH (luteinizing hormone) are the "conductors" of the menstrual cycle. When the ovaries become less sensitive, the brain increases their production to restart the machine.
As a result, their levels rise, sometimes sharply. A high FSH level is also an indicator of perimenopause, even if it is not enough to make a diagnosis alone. Because these hormones do not directly cause symptoms... But they do indicate a disruption or a potential transition phase underway.
DHEA, testosterone, cortisol: the silent but essential ones
Androgens (such as DHEA or testosterone) are less often discussed. And yet, their decline affects women's comfort, including:
- their energy;
- their concentration;
- their libido;
- their muscular strength.
Cortisol, the stress hormone, also tends to rise if the body struggles to adapt to all these upheavals. When the endocrine system is under pressure, the body prioritizes stress management at the expense of reproductive functions. A phenomenon known as "cortisol priority," which amplifies fatigue and sleep disturbances.
Quite a hormonal puzzle, isn't it? But understanding it is already a first step. Because it allows you to better decode your symptoms and get away from the idea that "it's all in your head." We'll tell you again: it's your body speaking in its own way.
What are the concrete impacts on the body of hormone variations during perimenopause?
While hormones orchestrate perimenopause behind the scenes, their fluctuations have very visible... and sometimes life-changing repercussions. Beyond irregular periods, the entire body reacts to this transitional phase.
Menstrual cycle becomes unpredictable
The duration of periods in premenopause is a whole story! Menstrual cycles get longer, get shorter, disappear for several months, then come back with a vengeance. Some women experience heavy periods, others vaginal bleeding between cycles. In short, you have to keep track—and this lack of guidance doesn't help.
Pain from head to toe
Breast pain (often linked to estrogen spikes, as a reminder) can become more frequent. Joint pain is sometimes added to this: it's rarely identified as hormonal, and yet it's very present! Some women report a feeling of morning stiffness or persistent discomfort in the knees, hips, shoulders... In short, we have pain all over, and it's not fun.
The urinary and pelvic system on the front line
Estrogen also influences pelvic muscle tone and urinary tract elasticity. Result:
- mild urinary incontinence;
- impression of a more fragile bladder;
- more uncomfortable sex.
Here are some intimate symptoms, which are rarely discussed, but which weigh heavily on daily life.
The famous “mental fog”
If only perimenopause were just a body thing... But no, that would be too easy! Many women also describe experiencing a kind of "brain fog." This is a difficulty concentrating, retaining information, or finding words. This isn't a sign of depression or burnout: it's a very real hormonal manifestation!
Fatigue that goes beyond simple “mental load”
Hormonal fluctuations, disrupted sleep, emotional and physical overstimulation... All of this can cause profound fatigue, not always relieved by a good night's sleep. Some women describe a loss of momentum, a need to withdraw, without being able to put it into words.
Invisible risks in the background
This period is also accompanied by an increase in:
- risks of cardiovascular diseases;
- of fracture risk;
- or even risk of cancer.
Nothing automatic, of course! But you should see this transition as a pivotal moment to take stock of your overall health, lifestyle habits, and prevention.
Perimenopause: how to support your body and your hormones?
Are your symptoms becoming overwhelming? Is your quality of life deteriorating? Don't stand by and do something! While perimenopause isn't an illness, it can require targeted support. Hormone therapy or natural alternatives? Here are the options, their benefits, their limitations, and the potential risks you should be aware of.
Hormone therapy for menopause (HTM)
Still too little known — even feared — hormone treatment remains the most effective option for relieving symptoms such as:
- hot flashes;
- night sweats;
- sleep disorders;
- or even genitourinary syndrome (discomfort during intercourse, dryness, repeated infections, etc.).
It is generally based on hormone replacement: estrogen alone or combined with progesterone, depending on the case. It can be taken orally, cutaneously (patch, gel) or vaginally (ovules, cream, vaginal ring).
The most recent studies (including that of Manson JE as part of the Women's Health Initiative ) have helped to qualify the fears linked to the risk of cancers and the risk of cardiovascular diseases. How? By showing that the latter depend mainly on:
- of the starting age;
- of the treatment plan;
- and health history.
Hence the importance of a personalized approach that assesses the benefit-risk for each woman.
Alternative and complementary treatment
Some women can't—or don't want to—use hormone replacement therapy. And we understand why. In this case, other options can help relieve premenopausal symptoms :
- herbal food supplements (black cohosh, sage, red clover, maca, etc.);
- phytoestrogens, in conjunction with medical monitoring;
- targeted micronutrition;
- low-dose antidepressant treatment (sometimes prescribed for mood or sleep disorders);
- relaxation techniques (yoga, breathing, cardiac coherence, etc.).
Caution: Natural does not mean harmless! We advise you to always seek medical advice, especially if you have a family history of hormone-dependent cancers or venous thrombosis.
The importance of lifestyle
Whether there is treatment or not, lifestyle habits play a central role during this period. Regular physical activity helps to:
- protect blood vessels;
- preserve bones (and limit the risk of fracture);
- balance cortisol.
Also try to eat a balanced diet. This will help you better manage your calorie intake and avoid the decrease in energy expenditure typical of this phase.
Of course, we also don't forget emotional support, which is crucial during these transitional years!
In short, perimenopause marks a major hormonal transition in women's lives—sometimes silent, often confusing, but never trivial. Understanding its mechanisms and recognizing its signs is already taking back control of this period! Because no, it's not "in your head." It's in your body, in your hormones, and you have the right to be informed, accompanied, and supported.